At each provincial hospital in Papua New Guinea is a specialist centre. For survivors of gender-based violence, these centres provide a one-stop shop for medical treatment and counselling, as well as provision of referrals to safe houses or police services.
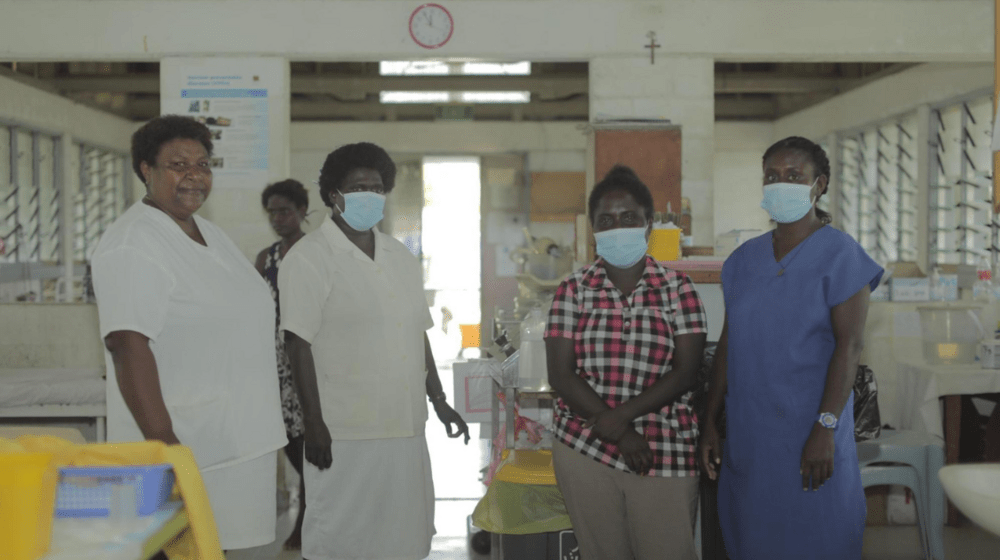
These centres are critical for the frontline response to gender-based violence in Papua New Guinea and at the heart of that response are the dedicated health professionals working to uphold the dignity and continued safety of survivors.
A Place of Comfort
At Buka General Hospital, Sr Michelle coordinates the Family Support Centre (FSC). She is a mental health nurse by profession and recognises the importance of maintaining a space removed from the busier hospital departments to provide adequate care for survivors of gender-based violence.
“GBV survivors come to the FSC quite traumatised,” Michelle shared. “If they come in through the outpatient department, there are many people there. So we need to provide a quiet place so that they can feel more comfortable, especially to allow us to provide that psychological first aid.”
The FSC also refers survivors to safe houses and, for girls and boys under 18 years old, child protection services.
“This is for women and children who do not feel safe returning to their house or their community,” says Michelle. “I do counselling in the FSC, but I am currently the only one here providing that service. If there is a need for continuous counselling, I refer them to the safe house where they are able to provide that.”
In addition to psychological first aid and counselling, Michelle conducts medical examinations, administers medication, and prepares medical reports. Following advocacy from UNFPA, these services are provided free of charge at the FSC. This is an important element to help survivors’ access to life-saving services. Patients may be charged if receiving care from the outpatient department or other parts of the hospital.

“We can refer survivors to law and justice services,” she says. “If the survivor wishes to take the case to court, the medical report is very important.”
These referral pathways are essential for survivors to avail themselves of long-term support. But they are just one part of the critical role of FSCs. For survivors of sexual violence, the FSC administers medical care for the prevention of sexually transmitted infections, including HIV.
Long standing capacity development from UNFPA Papua New Guinea, with support from Zonta International, has strengthened Michelle and her colleague’s capacity to deliver survivor-centred medical care for survivors and help the FSC meet the required standards.
For Michelle, the impact has been immediate.
“We recently had a case. A woman who was a survivor of sexual abuse,” said Michelle. “The training helped us understand the criticality of the timing for administering the post-exposure prophylaxis she needed. The two immunisations we give are very important in terms of any sexual violence cases.”
“With the prophylaxis, we need to give this within 72 hours. That is very important for preventing HIV infection, STIs, and pregnancy.”

Shared Responsibility for Care of Gender-based Violence Survivors
“This training was an eye-opener for many of us at the hospital,” reflected Sr Luanna. “This has really helped us step up our care for gender-based violence survivors.”
Sr Luanna is an experienced intensive care nurse now serving as the clinical supervisor at Buka General Hospital. She is responsible for ensuring all nursing staff, including those in the FSC, perform procedures according to standards and maintain the highest standards of care. It is a demanding role in the resource-strained environment.
“Initially, I knew nothing about the referral pathways for gender-based violence survivors and what needs to be done straight away for these patients,” she shared. “I took it for granted that there were people in specific positions in the hospital that knew what to do and where to send survivors. Through this training it came to my attention that even the staff in those positions were not too sure about how to refer GBV survivors to where they were supposed to go.”
“So I felt that this training has helped me realise what I can do in the hospital setting for clients who come in with this issue.”
Sr Luanna was joined in this training by the doctor in charge of the outpatient clinic, health extension officers, and nursing officers. She said that the impact of the training was felt immediately. Changes were put in place, including the roll out of the new referral pathway.
Sustaining Change
With the new referral pathway now up and running within the hospital, women and children experiencing violence have more avenues to receive the help they need. Survivors who attend the outpatient clinic out of hours can now receive the medication they need and stay at the hospital until the Family Support Centre opens and they can receive psychological first aid and further referrals to safe houses.
For Luanna, seeing the numbers increase is a testament to the training they received and the actions they are taking as a team of healthcare professionals.
“When the training finished, Sr Kalabai was flooded with GBV survivors,” shared Sr Luanna. “She recognised more GBV survivors and that in turn has made us realise she needs help at the Family Support Centre to deal with these cases.”
“I feel we specifically need someone with a social work background looking after a GBV unit to ensure the right help is given to clients when they need it. I am thankful that the Zonta funded UNFPA programme, has helped us realise the importance of this issue.”
UNFPA continues to work with staff at Buka General Hospital, and with FSCs around the country, to improve health services for women and girls experiencing violence.
Gender-based Violence in Bougainville
According to the Papua New Guinea National Statistical Office, 54% of women from AROB have experienced physical or sexual violence from their partner within the past year. Only 1 in 5 women in AROB who have ever experienced intimate partner violence sought help to stop the violence.
Nationally, 3.3% of women who experience intimate partner violence seek help from healthcare providers. However, with over 50% of those who experience such violence incurring serious injury, it is likely that there are women presenting to health services with injuries sustained from intimate partner violence who don’t report the true cause of their injury.
Recognising signs of intimate partner violence is important for all health workers in the hospital because most survivors are hesitant to share their experiences or to present directly to the FSC. With specialised training, health workers can strengthen their approach to patients they identify may have experienced such violence to ensure that survivors feel safe and can learn about services and supports available to them.
Acknowledgements
UNFPA would like to express our sincere appreciation to everyone involved in the project partner organizations, and government representatives, and others who helped make the project a success.
Without the generous support from Zonta International Foundation and their unwavering commitment to improve the lives of women and girls and ending gender-based violence in Asia and the Pacific Region, these significant achievements