You are here
“We have to be one with them”
“We have to be one with them”
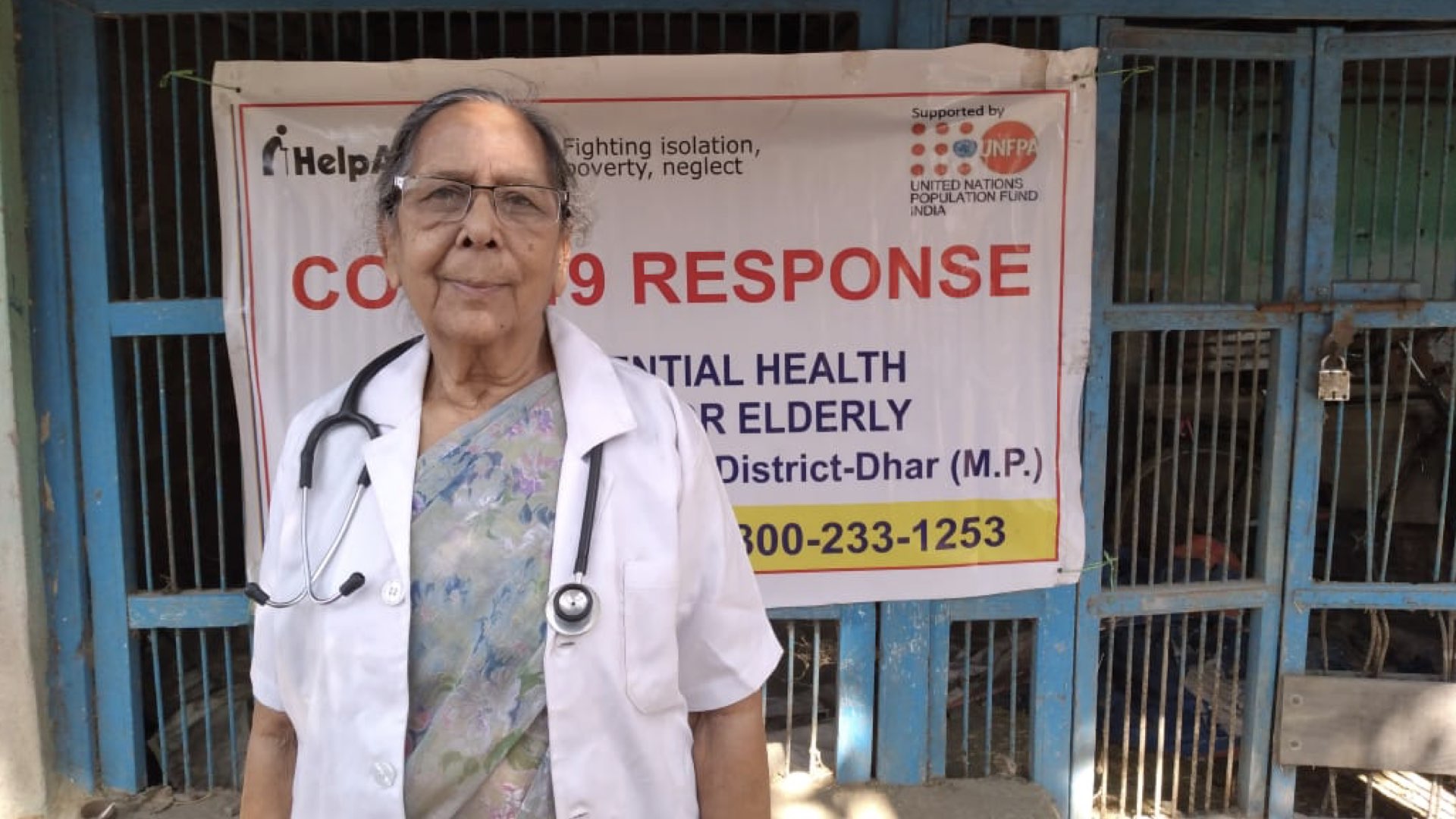
Dr Usha Vaidya is 84 years old and leads rural outreach teams to deliver medical services to older people through the Mobile Health Unit in Indore, a city in the central Indian state of Madhya Pradesh. She says older people in her region were already isolated before the pandemic, but with financial stress and the medical system overwhelmed by the virus, COVID-19 has made them even more vulnerable. Usha and her colleagues have adapted protocols and sourced supplies to deliver mobile health services to older people in rural areas.
Usha reports that the pandemic has been a stressful time for older people in the villages she visits. “There were no doctors available because most of the doctors were employed on COVID-19 duty,” she says. “The people were waiting for advice from somewhere.”
Older people were not coping well during the lockdown, with a crippling reduction in services and rumours related to infection and the symptoms of the virus. “They were ready to purchase medicines from outside because we would not have been able to give them medicine for a month or more,” Usha says. “As it is, there is a high incidence of poverty in villages. This poverty results in lower levels of health awareness and education.” She and her colleagues have to explain to patients the advantages and disadvantages of various kinds of treatment for diabetes and hypertension, and she encourages them to think about the consequences if their condition does not improve quickly.
Usha began her work as a doctor in 1963 and spent several years in the Indian Army before she got involved in rural outreach and elderly care. “I was working with some mobile units,” she says. “I wanted to put my extra time to productive use, so I started working in this area.”
“So many times there is no medical help available. Whatever we can give, older people are really appreciative.”
For the past five years, Usha has been going to villages in Madhya Pradesh and providing house-by-house treatment for older people. “So many times there is no medical help available,” she says. “Whatever we can give, older people are really appreciative.”

With high incidence of hypertension, diabetes and stroke, Usha says, ensuring that patients take regular medication is critical. Part of her work is convincing older people to take medicines consistently. This requires patience and an egalitarian approach. “It is difficult to convince them that taking their prescribed medicines regularly is the most important thing they can do for their health,” she says. “Gradually, they found that the people taking medicines continuously were improving, so they started coming to the mobile unit. It was very satisfying.”
“It is difficult to convince them that taking their prescribed medicines regularly is the most important thing they can do for their health.”
Usha reports that government programmes supporting vulnerable groups with food and rent during the pandemic have helped ease the immediate burden. She says she is in awe of the ways people in rural communities get by with so little. Despite this resilience, the need she encountered was often great, especially in places with many older people but limited support.
“There was a great need for medical care in old age homes,” she says about recent outreach work. “We distributed things like a refrigerator, essential supplies and medicines.”
Over the years, Usha has become a consistent and trusted authority on rural health in the communities and in discussions with partners. When she began her career in medicine six decades ago, she felt there was little interest in rural health and elderly care. “The new generation is becoming interested in rural health,” she says. “Slowly and gradually, services are coming.”
For Usha, the key to connecting with rural communities is the way doctors approach their patients. “It is actually the psychology behind it,” she says. “If you talk to them as if you are from the city, you are superior, then it won’t work.”
“We have to be very patient with older people. We have to know what we are going to do medically, but psychologically we have to be one with them.”
Usha knows what it takes to connect and deliver quality care. She believes that listening is the most important part of her job. “We have to be very patient with older people,” she says. “We have to know what we are going to do medically, but psychologically we have to be one with them.”
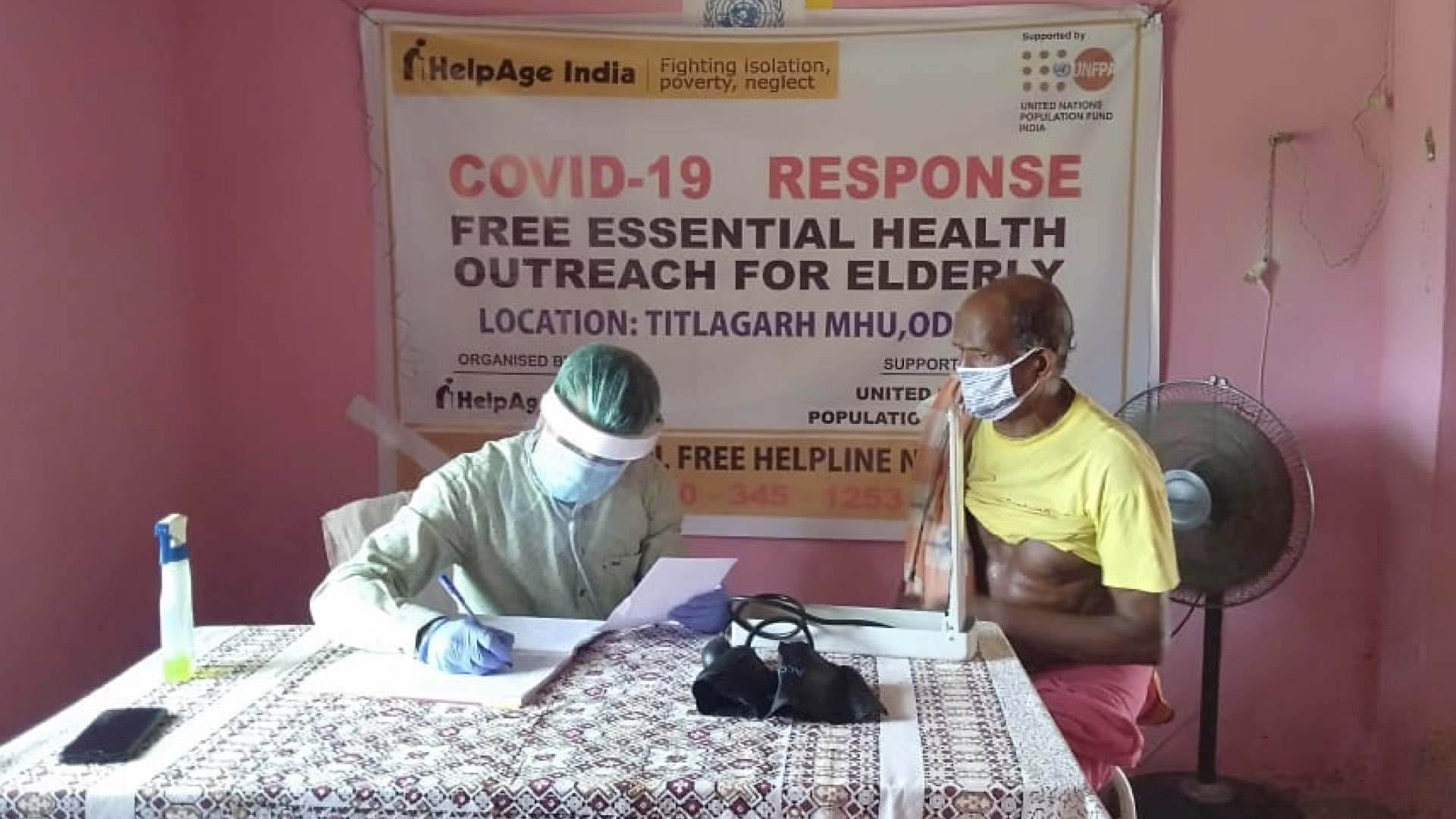
The outreach was made possible through a UNFPA–HelpAge India partnership to meet the challenges faced by older people in India in the context of COVID-19. With UNFPA support, HelpAge India reached more than 300,000 older people through different health interventions across 17 states.


